
Awarded Outstanding Value Health Insurance 16 years running
We’re proud to deliver outstanding value health insurance products designed to suit your needs. But don’t just take our word for it.

Hospital & Extras offer - Want 6 weeks free and up to $500 in gift cards?
Join and maintain eligible Bronze hospital and extras cover or above and you could get 6 weeks free plus 50,000 Live Better points (couples and families) or 25,000 Live Better points (singles and single parents) to redeem on rewards like gift cards. We'll also waive 2&6 month waiting periods on extras. New members only.€ Use promo code: 6WEEKSPLUS
Get a quote Find out more
Why choose Medibank private health insurance?
With over 45 years of experience, we understand what better health means.
Accident cover boost
Medibank members with hospital cover get the benefits of Gold level cover no matter what level of hospital cover you have, thanks to our Accident Injury Benefit.1
24/7 Medibank Nurse
Members with hospital cover can call our phone service to speak to a Medibank nurse about their health concerns at any time of the day or night.2

100% back on dental check-ups twice a year on eligible extras⁼
Here’s something to smile about – Medibank members with eligible extras cover for two months or more get 100% back on up to two dental check-ups every year, including x-rays, at any Members’ Choice Advantage dentist.=
100% back on optical on eligible extras±
At Medibank we think you deserve to see the world clearly. That's why when you join eligible Medibank extras you get 100% back on optical items at all recognised providers up to annual limits.±
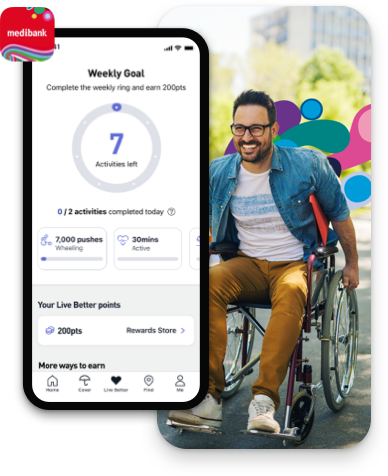
Live Better rewards
With Live Better rewards, you can earn points by tracking healthy actions. And if you're an eligible Medibank member with hospital or extras, these points can go towards rewards from select partners such as adidas and THE ICONIC, as well as select Apple products, extras limit increases or a $200 premium payment.3

Why choose Medibank Corporate cover
- Enjoy a corporate discount
- Choose how to spend your extras~
- 80% back on included extras^
- 100% back on dental check-ups twice a year on eligible extras=
Switching to Medibank has never been easier
1. Find your cover
We help you find the health insurance that best suits your needs.
2. Let us do the paperwork
Simple and easy. We’ll cancel your old membership for you.
3. No waiting periods again
There’s no need to re-serve waiting periods you’ve already served with your old fund.4

Need some help navigating health insurance?
Things you should know
1 For Accidents that occur in Australia after your cover starts. Must seek medical treatment within 7 days, and receive hospital treatment within 12 months, of the Accident occurring. Excludes claims covered by third parties and our Private Room Promise. Out of pockets may apply.
2 OSHC members should call the Student Health & Support Line on 1800 887 283.
= Eligible members on Medibank extras (excluding Healthy Living Extras and Gold Ultra Health) can claim a maximum of two 100% back dental check-ups per member, per year at a Members’ Choice Advantage provider (including bitewing x-rays where clinically required). For members on eligible extras, the first two check-ups do not count towards your annual limit. Members with Healthy Living Extras can get 100% back on one dental check-up each year at a Members’ Choice Advantage provider (including up to two bitewing x-rays, where clinically required) or at a Members’ Choice provider (excluding x-rays). Members with Gold Ultra Health can get 100% back on up to three dental check-ups at a Members’ Choice or Members’ Choice Advantage provider. Members’ Choice and Members’ Choice Advantage providers are not available in all areas. Two month waiting period applies. Some products may have other dental benefits, check your cover summary for details.
± Excludes Healthy Living Extras and select products that are no longer available for sale (for more information check your cover summary or check this page). Applies to prescription glasses and select contact lenses. Some glasses lens coatings and contact lenses are excluded. To find which specific items are included or excluded, call us on 132 331. 6 month waiting period applies.
3 Must be 16 years or over and have a valid Australian residential address to register for Medibank Live Better. Must be a Medibank member with hospital cover, extras cover, or hospital and extras cover, be up-to-date with premium payments and have signed up to Medibank Live Better with ‘My Medibank’ or have linked their MyMedibank account with their Live Better account to redeem rewards. Excludes Overseas Student Health Cover (OSHC), Ambulance only cover, ahm covers and other selected covers. Additional terms and conditions may apply to the redemption of a reward depending on the type of reward chosen. See full Medibank Live Better terms.
~ At recognised providers. Waiting periods and annual limits apply. Excludes optical.
^ Up to annual limits. Waiting periods apply. Excludes optical. Excludes Flexi 80 MC.
4 You need to join Medibank within 2 months of leaving your old fund, or waiting periods apply again. Also, benefits that have been paid under your previous cover will be taken into account in determining the extras benefits payable under your Medibank cover.
€ For new members on new memberships who join and start eligible combined Bronze hospital and extras cover or above from 22 April 2024 and who have not held Medibank health cover in previous 60 days (unless they are dependents coming off their parent’s cover). Must quote promo code ‘6WEEKSPLUS’ and set up direct debit when joining. Excludes Hospital only cover, Extras only cover, Basic covers, Corporate covers, Accident Cover, Ambulance Cover, Overseas Visitors Cover (OVC), Overseas Students Health Cover (OSHC), Overseas Workers Health cover, Travel Insurance, Pet Insurance, Funeral Insurance, Life Insurance & Income Protection, ahm covers and all corporate covers. Not available with any other offer. Medibank may end this offer or amend these offer terms and conditions at any time without notice. Medibank employees are not eligible for this offer.
6 weeks free terms: Must maintain direct debit and hold eligible cover for 42 consecutive days from the policy start date to get next 6 weeks free. The 6 weeks free will not be issued if you change to an ineligible cover, terminate your cover or suspend your cover during this period.
2&6 month waits waived on extras terms: 2&6 month waiting periods on extras waived. Other waiting periods apply (including 12 months on some dental services). If you're switching from another fund and you’ve used any of your current limits (at that fund), that will count towards your annual limits with us. If you've reached your limits at your previous fund you may not be able to claim straight away on extras.
Live Better points terms: Must maintain direct debit and hold eligible product for 42 consecutive days from the policy start date to receive Live Better points. The points will not be issued if you change to an ineligible cover, terminate your cover or suspend your cover during this period. Policyholder will require access to a smartphone and will need to download the My Medibank App. Policyholder will need to have registered a My Medibank account, sign up to Live Better via the My Medibank App and track any Live Better activity within 42 consecutive days from the policy start date. Policyholder must also maintain direct debit and continue to hold an eligible product for 42 consecutive days from the policy start date to receive the Live Better points. Must be 16 years or over and have a valid Australian residential address to register for Medibank Live Better. Live Better points could take up to 10 weeks from the policy start date to be loaded to the policyholder’s Live Better account. Singles and single parents will receive 25,000 Live Better points, and families and couples will receive 50,000 Live Better points.
Live Better rewards terms: Must be a Medibank member with eligible hospital cover, extras cover, or hospital and extras cover, be up-to-date with premium payments and have signed up to Medibank Live Better via the ‘My Medibank’ app to redeem rewards. Additional terms and conditions may apply to the redemption of a reward depending on the type of reward chosen. Read full Medibank Live Better terms here: https://www.medibank.com.au/livebetter/rewards/terms/
